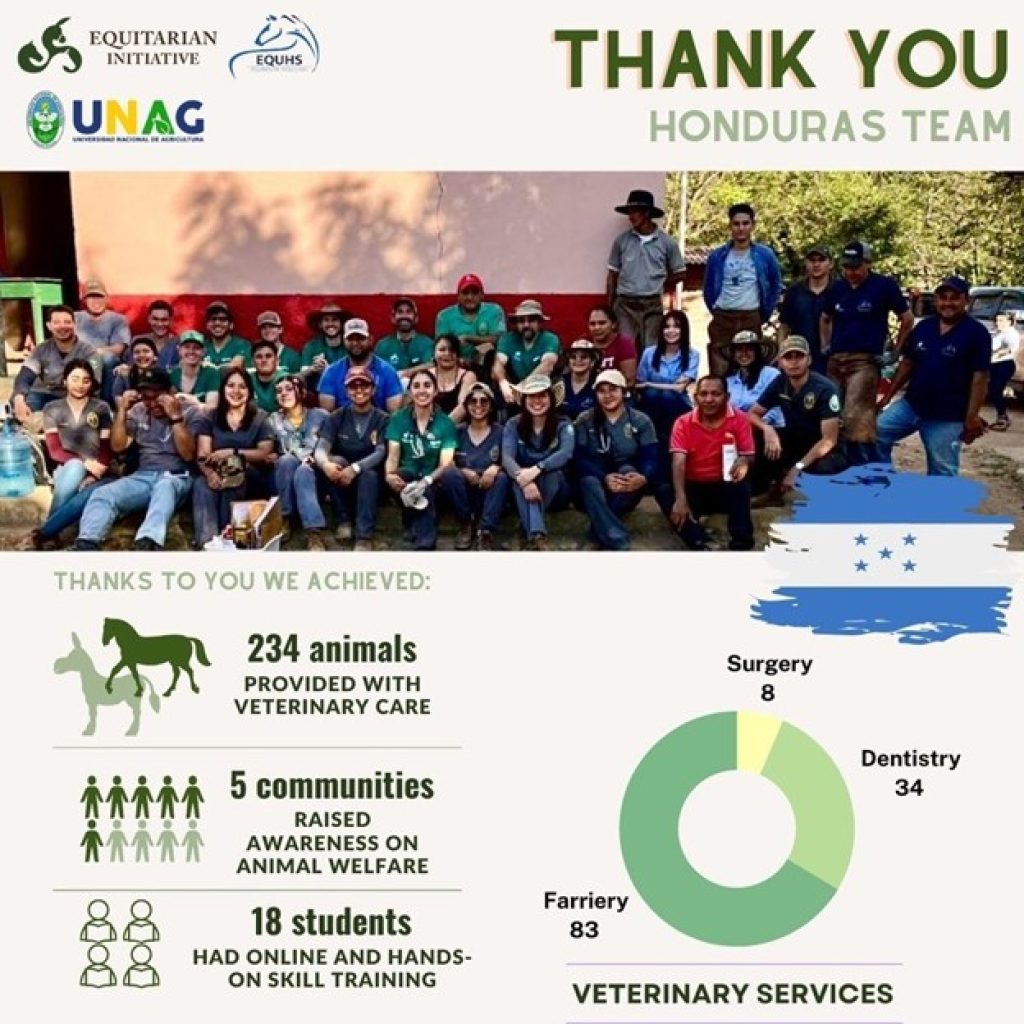
Dr. Baer in Honduras-Veterinary volunteer work with Equitarian Initiative
While most of you were hunkered down during the frigid week of February 8-15, I was warm and hard at work in Honduras. During this time, I was fortunate enough to have been selected for a volunteer veterinary trip with the Equitarian Initiative. Originally scheduled for November 2024, this trip was initially postponed due to tropical storms and flooding in the area.
The Equitarian Initiative is a non-profit organization providing philanthropic veterinary care for working horses, donkeys, and mules. Projects are focused in locations that lack access to basic veterinary care and work to align with local veterinary students and organizations to provide owner education. Conclusion of a successful project means that communities have been able to establish local care and no longer rely on outside help from EI. Current project locations include Haiti, Nicaragua, Honduras, Guatemala, Peru, Dominican Republic, Costa Rica, and the Pine Ridge Reservation in South Dakota.
After flying into Comayagua, Honduras, we headed almost 3 hours south to the Choluteca region. Each day involved setting up a clinic in a different community, as close as 30 minutes away or as far as a few hours away. Getting to our most remote clinic location involved a 1.5-hour drive, a river crossing by rowboat, and a 1.5-mile hike! We had an international group of 8 veterinarians and 18 Honduran vet students. EQUHS (Equinos de Honduras) a local group, worked closely with us during the trip as well. EQUHS helps EI partner with various communities, provides owner education and resources, educates veterinary students, and promotes establishment of animal welfare curricula. We also had local farriers working at the clinic sites every day.
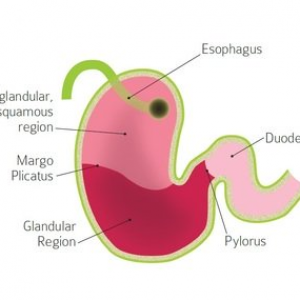
Each clinic day, teams composed of one veterinarian and two veterinary students were assigned to either triage, surgery, anesthesia, or dentistry services. There was also a registration team from EQUHS assigning numbers to the horses in order of arrival. The triage teams were responsible for initial intake exams on all horses. Under the supervision of their team vet, the vet students performed these initial examinations, including physical exams, body condition scores, dental checks, administration of rabies vaccinations and dewormer, and application of topical parasite treatments. Working in triage provided a great opportunity for client education (and for me to work on my Spanish!). It was excellent practice for the students to explain their exam findings to horse owners. From triage, horses requiring dentistry, farriery, or surgery were then moved on to those stations. Anesthesia teams were responsible for pre-anesthetic exams and medication calculations prior to surgery. At surgery, anesthesia teams were responsible for laying the horse down, monitoring anesthesia, and helping the horse recover after surgery. Surgery teams were set up primarily to provide castrations, but an additional surgical case required flushing and debriding a severe hock wound while the horse was anesthetized. Dentistry teams provided dentistry services including sedated oral exams, floats, and extractions.
My communication with the students was sometimes challenging due to my limited technical vocabulary in Spanish, but they truly did a great job throughout the week and benefitted from this opportunity to practice their clinical skills. Hopefully some of these students will consider future career opportunities in equine veterinary medicine.
The days were long and hot, leaving us physically and mentally exhausted, but also extremely fulfilling and gratifying. Some of the horse owners traveled great distances to get care for their equine partners, and they were appreciative and invested in the process. The whole experience provided me with a new perspective on equine veterinary medicine, and I am grateful to have had this amazing opportunity. I hope to volunteer with EI again soon!
For more information about the Equitarian Initiative and how you can help, check out the EI website, https://equitarianinitiative.org/